When the Network Vanishes: NYCEPPO Members Were Promised More Doctors — Instead, They’re Losing Thousands
How UnitedHealthcare’s network is silently shrinking, entire hospital systems are cutting ties, and its Optum clinics are closing — and why NYC workers and retirees were never told this could happen.
When the UFT and Municipal Labor Committee pushed the transition to the new UHC NYCEPPO plan, one promise was repeated over and over — the network will be bigger. We were told retirees moving to Florida or Pennsylvania would finally have more in-network doctors. We were told New Jersey and Pennsylvania commuters working in NYC would have easier access to hospitals near their homes. And we were told this would be an “upgrade,” not a sacrifice.
Months later, that promise has collapsed.
Entire health systems are walking away from UnitedHealthcare. UHC’s own Optum clinics are shutting their doors. And far from expanding, the NYCEPPO network is beginning to shrink — rapidly. The worst part? UnitedHealthcare’s provider counts disguise the damage. They don’t count doctors — they count locations, medical staff, and even the same provider multiple times if they list more than one specialty. So when a large hospital system or multi-specialty group leaves, UHC doesn’t just lose a few doctors on paper — they lose thousands of listed “providers” in a single blow.
And that’s exactly what’s happening now.
When a Whole Hospital System Walks Away
In Pennsylvania, Lehigh Valley Health Network (now under Jefferson Health) announced it is cutting ties with UHC by April of 2026, unless a deal is struck. LVHN said UnitedHealthcare has underpaid them by nearly 40% of agreed reimbursement rates since 2021 — making the contract unsustainable. This isn’t just one hospital: it’s 15 hospitals, thousands of doctors, specialists, imaging centers, rehabilitation facilities, and outpatient clinics across 10 counties.
For thousands of NYC workers and retirees who live in Pennsylvania and New Jersey and commute to work — the very people UFT claimed would gain more access — their providers will be out-of-network by April of 2026. UnitedHealthcare and LVHN are pointing fingers at each other. But patients are the ones caught in the middle, making impossible choices: stay with their doctor and pay out-of-network prices, or delay or abandon their care entirely.
John Hopkins Medicine: Now out-of-network
And the final chapter in this saga may be the one none of us anticipated. In August 2025, Johns Hopkins Medicine — one of the premier academic medical centers in the country — officially informed patients that it could no longer reach a contract with UnitedHealthcare, meaning nearly all of its hospitals and clinics in Maryland, Virginia and Washington, D.C. would be treated as out-of-network for UHC members as of August 25. For roughly 60,000 UHC-covered patients, this isn’t a minor disruption; it’s a full blow to access.
Hopkins says the fight was never just about money — it was about excessive prior-authorization demands, claim denials, and contract language that would tie care to profit rather than patients.
If an institution of Johns Hopkins’ scale can exit the network, it stands as yet another alarm bell for NYCEPPO members: no doctor, no hospital system is truly immune.
The network sold to you as “expanded” can shrink overnight — and your right to care, your continuity, your trust in the plan may evaporate just as quickly.
Meanwhile — UnitedHealthcare Is Shuttering Its Own Clinics
While hospital systems are cutting UHC loose, UHC is shrinking itself from the inside.
UnitedHealthcare’s subsidiary Optum Health — which runs clinics across multiple states — has quietly closed dozens of medical offices in New Jersey, Minnesota, Florida and beyond. Patients got sudden emails and phone calls: their doctor is gone, their appointment cancelled, their clinic permanently closed. In some cases, entire clinics serving primary care, pediatrics, cardiology, behavioral health, and geriatrics were wiped out in a single announcement.
In New Jersey alone, over 90 offices are closing and laying off hundreds of employees.
Medications and records will be interrupted. Pregnant women, cancer patients, and seniors are left scrambling for new doctors with almost no notice.
The Promise That Became a Lie
When NYCEPPO was introduced, the UFT said clearly: more doctors, more hospitals, wider national access — especially for retirees and members in New Jersey and Pennsylvania.
But three realities were never disclosed:
1. Network size was exaggerated from the start.
UnitedHealthcare inflates provider numbers by counting:
The same doctor multiple times if they list more than one specialty.
Individual office locations as separate “providers.”
Physician assistants, nurse practitioners, and even administrative medical staff in totals.
So when a large system like LVHN and John Hopkins leaves, UnitedHealthcare doesn’t just lose a few doctors — it loses thousands of entries it had counted as “providers.” What was sold as “A million+ providers nationwide” is now quietly shrinking, and members don’t find out until it’s their doctor who disappears from the directory.
2. There was never a disclosed guarantee of network stability once the change was approved.
Contracts between insurers and health systems renew annually or biannually. If UHC refuses higher reimbursement or hospitals reject lower payments — the contract dies. And NYCEPPO members, despite paying premiums through their labor, have no seat at that table.
3. The union bosses and City themselves have threatened to punish non-cooperating hospitals — by raising our copays.
In multiple spaces and FAQs, UFT and MLC leaders have stated that hospitals or provider systems they believe are “not collaborating” or “driving up costs” could face added penalties in the form of higher copays imposed on members who use them. In other words — to pressure hospitals, they are willing to transfer the financial punishment directly onto us, the patients. Not UHC. Not the City. Us.
This is cost-shifting disguised as “healthcare savings.” It’s a punishment model — and it turns members into leverage weapons against their own doctors and hospitals.
We’ve already experienced this over the last decade with much higher copays for urgent care and emergency room visits.
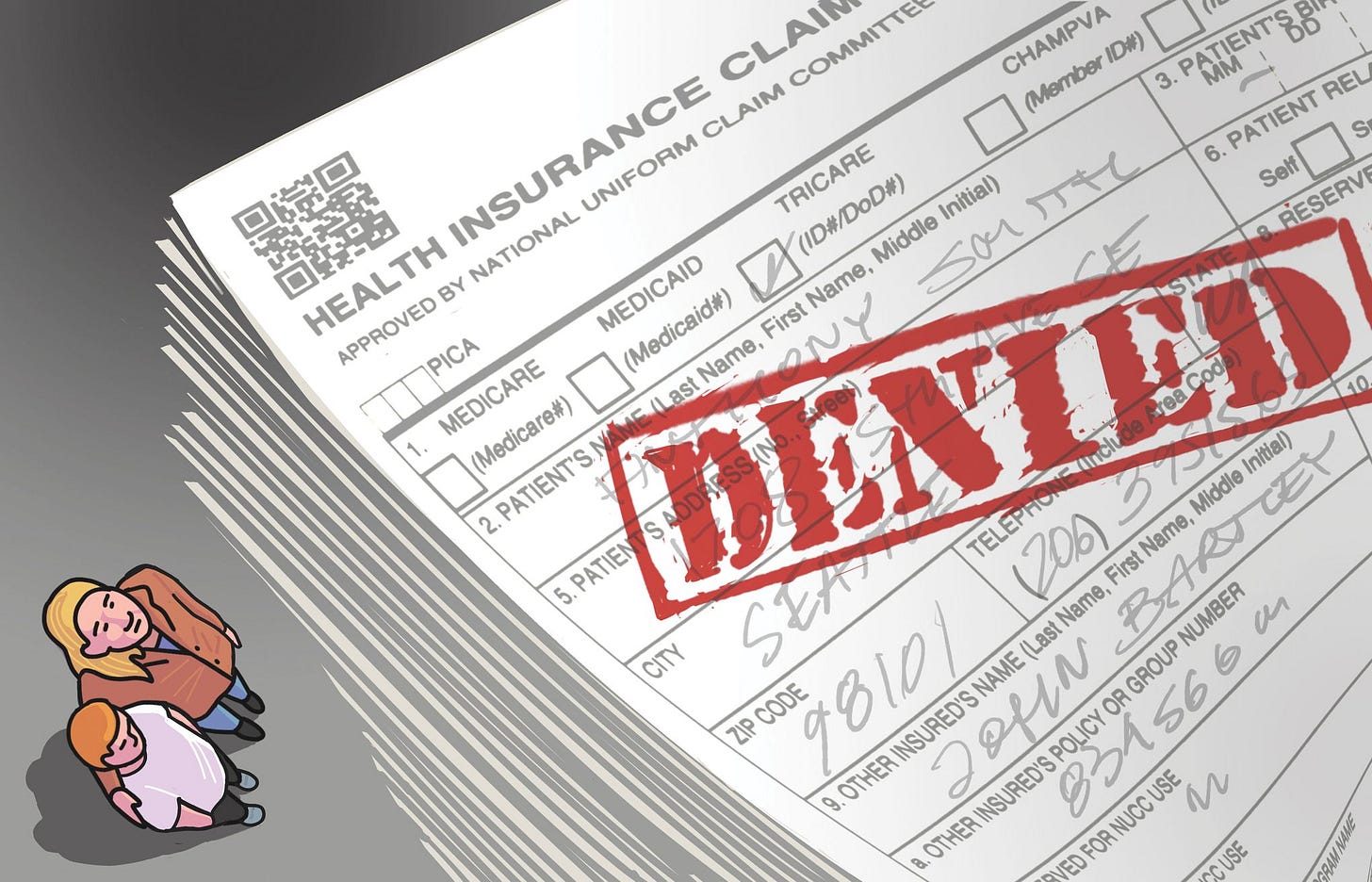
Next Comes the Denials
As networks shrink, another threat grows: denials of care.
UnitedHealthcare already leads the industry in treatment denials with 32% denial rate. Federal investigations have shown that UHC uses algorithms to auto-deny care for elderly and chronically ill patients — sometimes in seconds, without a doctor ever reviewing the case. Prior authorizations for MRIs, surgeries, physical therapy, and life-sustaining care are being rejected at staggering rates.
Fewer in-network doctors + more corporate control over authorizations = more patients delayed, denied, or pushed into debt. For NYCEPPO members managing cancer, diabetes, pregnancy, organ transplants, or long-term therapies, this is no longer a hypothetical threat. It’s here.
Call to Action — Before More Doctors Disappear
For UFT Members and Retirees:
Ask your doctors directly: “Will you still accept UHC NYCEPPO next year?”
If you live in PA or NJ, find out if your hospital system is negotiating with UHC or planning to withdraw.
Document your treatments, pre-authorizations, and specialist relationships now — especially if you’re in ongoing care.
Demand from your union: Was this network instability disclosed? Who monitors future contract terminations? Why are retirees losing doctors after being promised more?
For Union Delegates & Chapter Leaders:
Call for a resolution requiring the UFT to release the full unredacted UHC contract — especially any redacted network guarantee clauses. A
Demand transparency on out-of-network trends and denial rates under NYCEPPO.
Demand that the MLC share any agreements between them and the City that guarantee there will be no premiums in the next 5 years.
Push for hearings with the City Council, Comptroller, and State legislators on healthcare oversight and improvements Administrative Code 12-126, such as Intro 1096.
For Elected Officials:
Hold public hearings on network loss under municipal health plans and the risks union members and taxpayers will face in a self-funded plan run by the City of New York.
Require insurers to disclose when 500+ providers are about to go out-of-network.
Protect continuity of care for patients undergoing treatment when networks suddenly collapse.
We don’t lose our healthcare in one moment. We lose it hospital by hospital, clinic by clinic, denial by denial… until the plan we paid for exists only on paper.
This is the time to act — before more of us are told our doctors no longer take our insurance.



We need to call on all our local council members to vote for Christopher Marte
A bit off-top, but relevant:
One of our City Councilmembers, Julie Menin, who is Chair of the Consumer and Worker Protection Committee, has been touted by our prominent union bosses as also standing for healthcare oversight and transparency.
It's been very frustrating how CM Menin has kept silent while Unity and the Heads of MLC rushed to pass their seriously redacted NYCE PPO plan.
Any coincidence that both Garrido and Mulgrew have been strongly pushing for CM Menin to become the next City Council Speaker?
On the other hand, Councilmember Christopher Marte, who is also running for City Council Speaker, with a powerful platform to empower our lawmakers and us through securing more transparency within the City Council is getting pushed to the bottom by these same union bosses.